Fecal Incontinence
Are your bowel incontinence symptoms disruptive to your daily activities? Have the freedom to live your life!
You are not alone.
~20 million
adults in the United States suffer from bowel incontinence, also referred to as accidental bowel leakage.1,2
What is Axonics® Therapy?
Axonics Therapy is an effective solution for treating symptoms of bowel (fecal) incontinence, overactive bladder including urinary urgency incontinence, and urinary retention3.
Bowel Incontinence
Overactive Bladder
Urinary Retention
What Is Bowel Incontinence?
Bowel incontinence, or accidental bowel leakage, is a condition where people get sudden urges to pass stool and experience leakage of stool before they make it to the restroom.
Bowel Incontinence Symptoms
You may be suffering from bowel incontinence if:
Fecal Urgency
You experience sudden urges to pass stool
Urgency Fecal Incontinence
You experience an inability to stop the urge to pass stool
Passive Bowel Incontinence
You experience leakage of stool with activity or without awareness
Did you know that patients can suffer from dual incontinence?
Dual incontinence is when a patient is experiencing both bladder and bowel control symptoms.

Your journey to find the treatment solution that works for you
-
CONSULT WITH YOUR DOCTOR
Discuss your symptoms
Start a baseline bowel diary
Undergo recommended diagnostic tests
Discuss treatment options -
INITIAL TREATMENT
Diet changes
Sphincter and pelvic floor exercises
Over-the-counter antidiarrheal medications
Pessary -
ADVANCED THERAPIES
Minimally Invasive
- Sacral Neuromodulation
Invasive
- Surgical Sphincter Repair
Bowel Incontinence Patient Care Pathway
Your doctor and his or her clinical team will follow a patient care pathway, which is a roadmap of the different treatment options available to you. The pathway starts with conservative treatments and then moves on to the advanced therapies.
No symptom improvements?
Don't give up!
Follow up with your doctor to discuss advanced therapy options
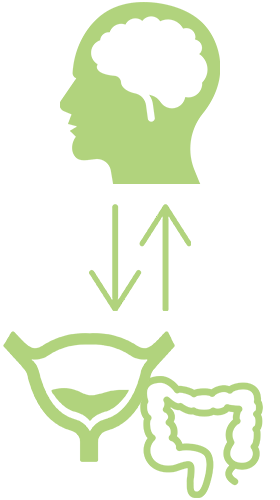
How does Axonics Therapy work?
Axonics Therapy provides gentle stimulation to the nerves that control the bladder and bowel, which can restore normal control and result in symptom improvement.
The Evaluation Step: To see if Axonics Therapy is right for you, you will undergo a short period of therapy using a temporary system. The evaluation period allows you to experience the level of symptom relief the therapy may provide before you commit to long-term therapy.
Long-term Therapy: If you and your doctor determine that Axonics Therapy is right for you, you will have an outpatient procedure where the miniaturized Axonics implant is placed just beneath the skin in the upper part of your buttock.

Clinically Proven. Patient Approved.
Backed by clinical studies, Axonics Therapy is clinically proven to regain bladder and bowel control and deliver clinically meaningful improvement in quality of life.
At 2-Years,
of patients had ≥50% reduction in FI symptoms 4
of patients were satisfied with the therapy for FI symptoms 3
of patients reported discomfort at the implant site 3